9 Thyroid Tests You Need To Know If Your Thyroid Is Healthy
Today’s mainstream clinical practices surrounding the detection and treatment of thyroid conditions are lacking. This predicament has left many thyroid sufferers without answers. Inadequate lab testing along with a huge reference gap in lab ranges leaves many thyroid conditions undetected and untreated.
It is estimated that 20 million Americans have some form of thyroid disease; these numbers continue to increase each year.
Nearly 60% of those with thyroid disorders are unaware of their condition (1).
Undiagnosed thyroid conditions put patients at risk for additional serious conditions, such as heart disease, infertility, osteoporosis, and weight gain/loss (1). Other common thyroid associated issues include, but not limited to, poor fat digestion, gallstones, fatigue, brain fog, constipation, diarrhea, infertility, and joint pain.
Pregnant women with hypothyroidism and subclinical hypothyroidism have a higher risk of miscarriages and have a greater chance of giving birth to children who have congenital defects and/or developmental conditions (1).
When mainstream testing standards finally do detect thyroid disease, an affected individual has likely had to suffer for a long period of time. Often, thyroid conditions are not detected until they have reached the full-blown disease stage. Early detection would undoubtedly improve clinical outcomes (2).
Today’s Standard Lab Tests and Ranges
It is common practice among mainstream medical professionals to measure the thyroid-stimulating hormone (TSH) with bloodwork to assess thyroid function. However, TSH is not an accurate marker for thyroid function when measured alone. Even with the addition of one or two thyroid hormone markers, it is still not enough information to confirm that there is or is not a thyroid condition present.
These standards need to change, but until then, there will be many who suffer for years, if not an entire lifetime, with an untreated and undetected thyroid condition.
Thankfully, there are alternative or holistic healthcare professionals who understand this issue and have pursued further education on the detection and diagnosis of thyroid conditions, but we need more education to support the millions struggling with thyroid-related illness today.
Thyroid Hormone Influence in the Body
Thyroid hormone output is controlled by the stimulation of TSH in a healthy functioning thyroid. (Note the word “HEALTHY,” as a diseased thyroid will not be able to generate adequate amounts of thyroid hormone.) The thyroid hormone releases from the thyroid gland in response to TSH. These thyroid hormones are called Thyroxine (T4) and Triiodothyronine (T3).
Many processes within our body will not function as they should without adequate thyroid hormone. In fact, it is believed that every cell in our body has thyroid hormone receptors.
When thyroid hormone is present, it is transported into the cell where it binds to a nuclear receptor. This then initiates a process called transcription. Transcription is responsible for the reading of genetic material that can then be translated into specific proteins that can be used for physiological function throughout the body.
Since T3 activates transcription, the processes that T3 are specific to do not occur if T3 is not present. An example of this would be myosin. Myosin is a cardiac protein responsible for increasing contractility of the heart. Adequate T3 is needed for the production of myosin. A lack of myosin results in reduced contractility of the heart muscle and ultimately, results in the cardiac complications that may be seen with hypothyroidism.
Thyroid Hormones Help Regulate:
Basal Metabolic Rate (BMR)
Heart rate
Body weight
Muscle strength and control
Central and peripheral nervous systems
Bone maintenance
Fat digestion and lipid levels in the blood (increased cholesterol, LDL and/or triglycerides can be indicative of low thyroid hormone)
Menstrual cycles
Mood
Breathing rate/rhythm
TESTING FOR THYROID FUNCTION
Given the importance of thyroid function, it is essential to properly test the function of the thyroid. In order to get an accurate assessment, the following laboratory blood markers should be tested:
TSH
T4
T3
Reverse T3
Free T4
Free T3
T3 Uptake/TBG
Thyroid Peroxidase (TPO) Antibodies
Thyroglobulin (Tg) Antibodies
Additional Testing
If hyperthyroidism is suspected:
TSH Antibodies
Thyroid Receptor (TR) Antibodies
Imaging:
Thyroid Ultrasound
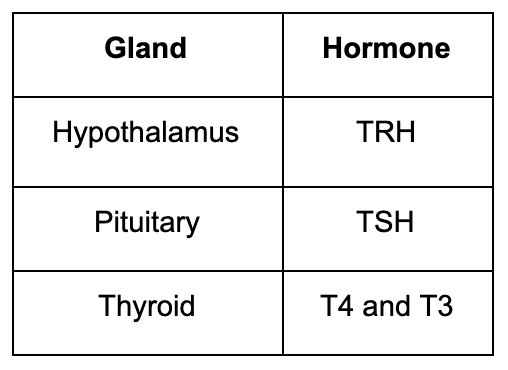
Test 1: TSH
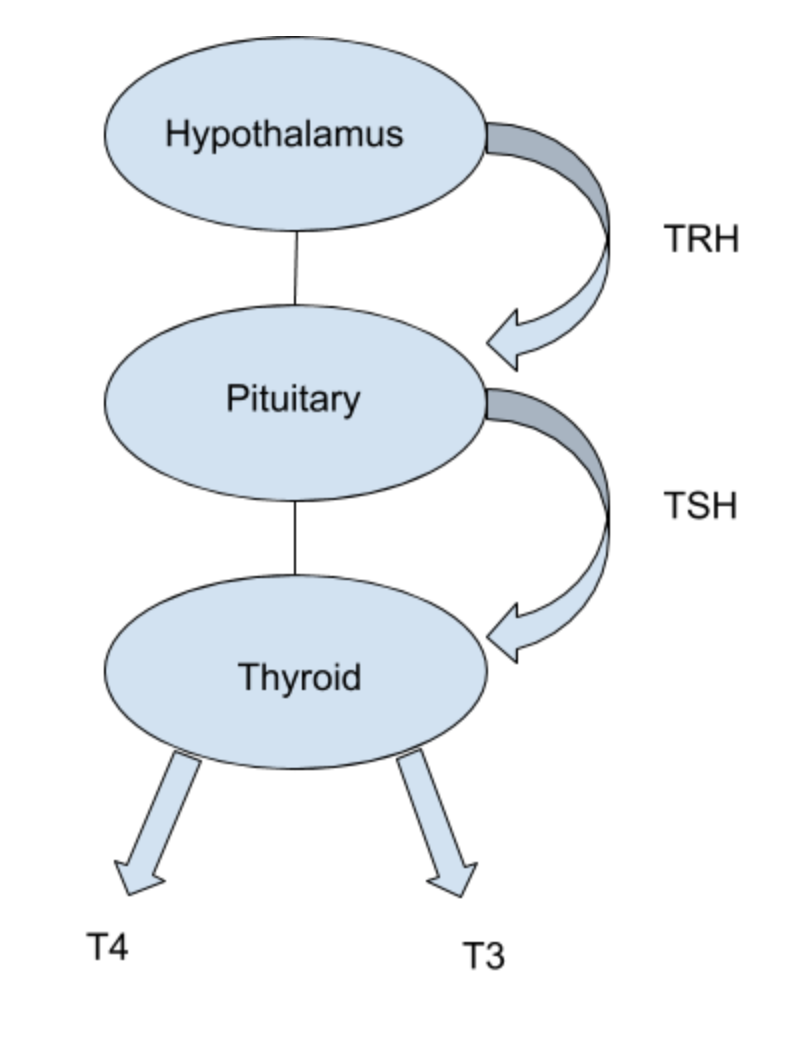
The demand for thyroid hormone output from the thyroid is controlled through a feedback loop. The hypothalamus and the pituitary are both a part of this loop.
As blood levels of thyroid hormone decrease in the blood, the hypothalamus releases thyroid releasing hormone (TRH) which signals to the pituitary to release thyroid stimulating hormone (TSH).
The TSH then acts upon the thyroid, signaling the need for an increase in thyroid hormone output (T4 and T3) from the thyroid.
In a perfect scenario, an increase of TSH results in an increase in thyroid hormone output.
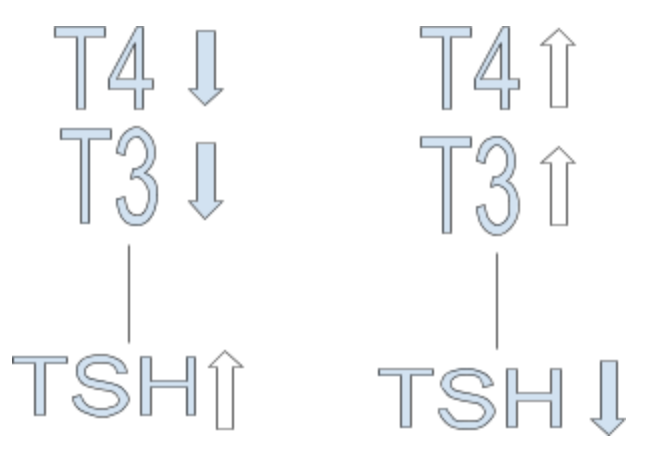
A decrease in TSH results in a decrease in thyroid hormone output. Once the body reaches a sufficient output in thyroid hormone, TSH should respond accordingly by either lowering (when there is enough hormone) or rising (when there is not enough).
This inverse relationship between TSH and thyroid hormone is why a high TSH can be seen in cases of hypothyroidism (low thyroid hormone output) and a low TSH can be seen in cases of hyperthyroidism (high thyroid hormone output).
Unfortunately, this perfect scenario is not how it always works out in real life. TSH is not always so intuitive.
Reasons Why You Need to Have More Than Just TSH Tested:
1. You can have a TSH that is well within lab range and still have low thyroid hormone output. TSH is not a direct measurement for thyroid hormone and may not reflect actual thyroid function.
2. A malfunctioning Hypothalamus-Pituitary-Adrenal or HPA axis can result in a poor TSH feedback loop.
3. Literally, any other thyroid marker indicative of dysfunction can be out of lab range, and this may or may not be reflected in TSH. In fact, this is very common.
4. TSH measurement can be within lab range in early stages of thyroid disease. This is where measuring thyroid hormones and antibodies, perhaps even a thyroid ultrasound, can be helpful.
5. In autoimmune conditions, the thyroid is commonly destroyed slowly over time. This cannot be reflected by TSH until a significant amount of thyroid tissue has been destroyed from relapsing autoimmune attacks on the thyroid gland.
6. Lab ranges are very forgiving, they are based on the averages of the local population. This does not mean it’s an optimal range, just comparative figures. TSH can absolutely be within lab range in an individual with thyroid disease.
7. With thyroid hormone replacement, TSH is not an accurate measurement for adequate dosing. Thyroid hormones need to be measured as well.
TSH Upper Limit:
There is much debate among researchers and clinicians as to what the standard upper limit range for TSH should be. Several parties believe that it should be lowered. One reason being that when risk factors for thyroid disease are excluded, the upper reference limit is considerably lower in healthy individuals than the standard lab range.
In 2002, researchers published results of a large sampling of the U.S. population. They determined that the mean TSH value of healthy individuals was 1.5 mlU/L (3).
Another study looked at 870 individuals that had been deemed healthy, based on TSH alone. They found that only 453 of the individuals actually had healthy thyroids when evaluated according to the National Academy of Clinical Biochemistry (NACB) guidelines, which included measuring thyroid hormones and utilizing ultrasound imaging (4).
NACB has recommended an upper limit of 2.5 mlU/L for TSH.
Dr. Mercola, New York Times bestseller and functional medicine doctor, states that TSH should be between 1.0 and 1.5 uIU/mL.
At Genesis Performance Chiropractic, we consider a healthy TSH to be 0.5 - 1.5 uIU/mL despite the local lab range listed as 0.45 – 4.5 uIU/mL. Keep in mind, we adhere more to a functional lab range. There is usually wiggle room for numbers as long as the whole picture makes sense and the person feels well. In our experience, we have seen suboptimal thyroid hormone markers with a TSH of 2.0 uIU/mL.
Summary: TSH is a pituitary hormone that stimulates the thyroid to make thyroid hormone. It is not an accurate test alone for thyroid function. TSH should be in the range of 0.5 - 1.5 uIU/mL. Other thyroid markers also need to be taken into consideration.
Tests 2 and 3: T4 and T3
When TSH is stimulated, both Thyroxine (T4) and Triiodothyronine (T3) are released from the thyroid gland. Both are bound by carrier proteins. T4 is the storage or inactive form of thyroid hormone and makes up about 93% of the thyroid hormone output. T3 is the active form and makes up about 7% of this output.
Thyroid Hormone Conversion
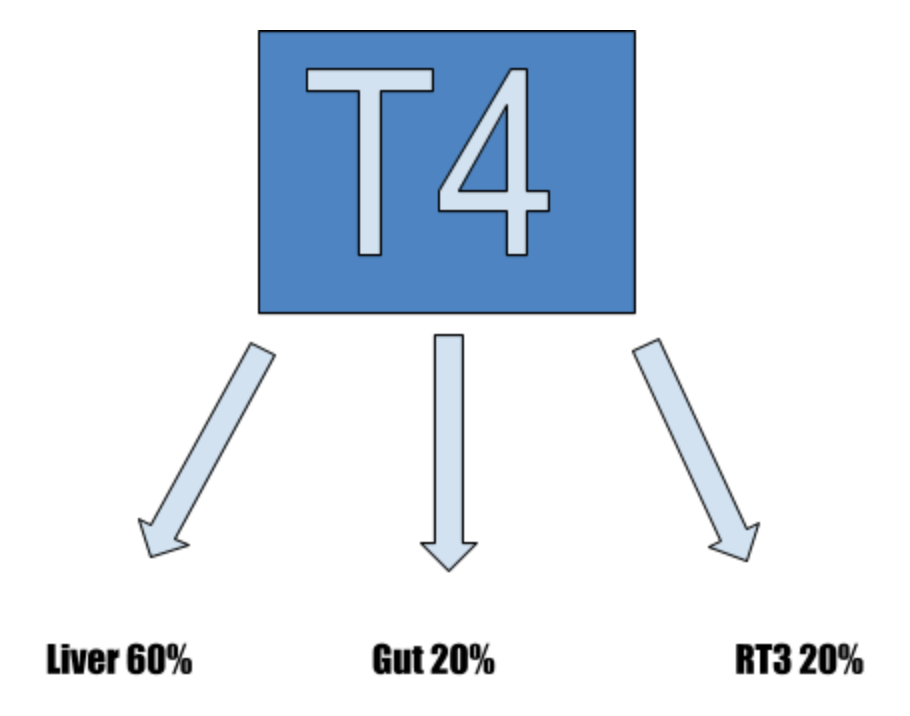
As thyroid hormone circulates peripherally, T4 is converted to T3 by an enzyme catalyst called 5’ deiodinase. T4 circulates through the bloodstream it is converted at different points.
The largest amount (60%) of conversion occurs in the liver. A healthy functioning liver is a large piece to ensuring conversion.
The GI tract converts T4 into T3 sulfate (T3S) and triiodothyroactetic acid (T3AC) until it enters the digestive tract and is acted upon by intestinal sulfatase. It then becomes T3. It is responsible for approximately 20% of T4 to T3 conversion. This is yet another reason to have a healthy microbiome.
Another portion (approximately 20%) is converted into reverse T3 (RT3). This is an inactive form of T3. In cases of illness or extreme stress, the conversion of RT3 can increase, Not only does it not provide the active effects of T3, but it also competes at the nuclear receptor sites with T3. This means a lowered ability for T3 to elicit its effects.
Test 4: Reverse T3
This test is not commonly ordered, because most doctors do not think it is necessary, as they are not trained to interpret it. However, this test is highly valuable.
Higher than normal RT3 (inactive hormone) means less T3 (active hormone). This is a problem, because high RT3 levels will slow down metabolism and reduce thyroid function. This can result in the patient feeling hypothyroid.
When RT3 is greater than 15 ng/dL, we start investigating why this number is elevated. Once the source is addressed, the RT3 will start to fall back into a normal range.
Reverse T3 becomes elevated with:
Stress (high cortisol)
Trauma
Inflammation
Infections
Toxicity
Zinc deficiency
Selenium Deficiency
Certain medications
Summary: RT3 should be less than 15 ng/dL. A lab value higher than 15 ng/dL can indicate some form of stress on the body. RT3 will normalize once the root issue is addressed.
Tests 5 and 6: Free T4 and Free T3
Remember that both T4 and T3 are bound by carrier proteins. Because of this, they are unable to be used by the cells until they become what we call “free.” Researchers do not know exactly when this happens.
The free thyroid hormone is able to bind to the nuclear receptor to be utilized by the cells for metabolic purposes. These free thyroid hormones are called free T3 (FT3) and free T4 (FT4).
Test 7: T3 Uptake & TBG
T3 uptake or Thyroxine-binding-hormone (TBG) should be ordered to help access the amount of carrier protein in the blood. These two tests measure differently, but give similar information.
Remember: Carrier proteins are those that attach to the thyroid hormone released from the thyroid (T4 and T3). When they lose the protein, they are called free T4 and free T3.
T3 Uptake
The T3 Uptake test is a way for practitioners to measure the amount of sites available for thyroid hormone to bind to carrier proteins for transportation. It is an indirect measurement of the amount of thyroxine binding proteins.
T3 Uptake is typically measured as a percentage. The lab range is typically 24-39%. Functional range is about 28-38%.
T3 Uptake will be low in cases where there is excess estrogen (estrogen dominance) or even if there is low thyroid hormone but normal or adequate levels of estrogen
T3 Uptake will be high in cases where testosterone levels are elevated. This could be found in conditions like PCOS, insulin resistance, hirsutism and the intake of testosterone hormone.
TBG
TBG makes up a majority of the proteins that transport thyroid hormone throughout the body. High levels of TBG will result in lower free hormone levels. This decreases the amount of hormone that is able to enter the cells (FT4 and FT3). Therefore, it can result in hypothyroid symptoms even with adequate thyroid hormone output. T3 Uptake and TBG have an inverse relationship. Therefore, you will have high TBG levels when you have low T3 uptake and low TBG levels when there is high T3 uptake.
Tests 8 and 9: Thyroid Antibodies (TPO, Tg)
Elevated thyroid antibodies can be found in thyroid diseases like Hashimoto’s and Graves. Lab high antibodies are needed for an autoimmune diagnosis, although an autoimmune disease of the thyroid gland can be present before thyroid antibodies are lab high or even detected.
This mechanism begins when the body’s own immune system creates antibodies to thyroid tissue. There are many stressors that are thought to induce this response.
Some Mechanisms That Can Lead to Thyroid Antibody Production:
Transfer of antibodies from from the mother in utero (6)
Dysbiosis (Leaky Gut) (7)
Infections (8) (EBV(9), Bartonella, Lyme, Yersina, H. Pylori (10), etc.)
Environmental Toxins (mold, heavy metals, chemicals) (11)
Stress (emotional and/or physical) (12)
Hashimoto’s
Iodine deficiency is the most common cause of hypothyroidism worldwide (13). However, autoimmune thyroid disease is the most common cause of hypothyroidism in the United States (14). This form of autoimmunity, known as Hashimoto’s, is 5-10 times more common in women than men (15) and the incidence increases with age.
Hashimoto’s Antibody Tests:
· Thyroid Peroxidase (TPO) Antibodies
· Thyroglobulin (Tg) Antibodies
Additional Tests- Grave’s Disease Antibodies:
Grave’s disease is marked by the overproduction of thyroid hormone due to an autoimmune process on the thyroid gland.
Grave’s Disease Antibody Tests:
· TSH Antibodies (16)
· Thyroid Receptor (TR) Antibodies
· Thyroid Peroxidase (TPO) Antibodies
· Thyroglobulin (Tg) Antibodies
Additional Test: Thyroid Ultrasound
Thyroid ultrasounds are a very effective diagnostic tool. They provide a high resolution image of the gland. Ultrasounds show evidence of thyroid dysfunction before any lab work does. Abnormal nodule findings can indicate a need for further testing.
Thyroid ultrasounds are used for:
A diagnostic tool for early detection of thyroid disease
Follow-up for abnormal thyroid blood work
Abnormal findings in physical exam of the neck (17)
Thyroid ultrasounds will show:
Swelling (indicative of thyroiditis or an autoimmune condition)
Blood flow throughout the gland
Abnormalities (cysts, nodules, tumors)
Nodule features (some features strongly correlate with a benign nodule while others correlate with cancer) (17)
Thyroid disease lies at the root of many health issues but using these testing methods will reveal and heal so individuals do not have to suffer as long. Please reach out if you have any questions or want to get tested.
Works cited:
Anca Staii, e. a. (2010). Hashimoto thyroiditis is more frequent than expected when diagnosed by cytology which uncovers a pre-clinical state. Thyroid Res., 11.
http://clinchem.aaccjnls.org/content/clinchem/51/8/1480.full.pdf
https://academic.oup.com/jcem/article-abstract/42/1/197/2685319?redirectedFrom=fulltext
https://www.tandfonline.com/doi/full/10.3402/mehd.v26.26191@zmeh20.2015.26.issue-s2
https://www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284
https://www.radiologyinfo.org/en/info.cfm?pg=us-thyroid#common-uses